During this time of COVID-19, social distancing, and schools being virtual for the time being, I know parents are struggling with keeping their children on task, engaged with their school work, and not pulling their own hair out of their heads. While as a physical therapist I don’t have all the answers to help with keeping your children on task, within my scope of practice I CAN offer guidance on the importance of flexible seating/standing options for your at home classroom space as well as which options may be the best for you to invest in to help your children thrive.
What is Flexible Seating?
Flexible seating is a concept in the school system which is getting increasing recognition and use in many classrooms. It encourages the idea of allowing children to sit where ever they want - basically getting rid of the “students sit in straight lined desks” idea that WE all grew up with. With this new model of seating also offers students a variety of chair/desk options to chose from as well around the classroom. From balls, to the floor, to a traditional desk, to a standing surface, teachers are attempting to offer “flexible” choices for their students in order to promote learning and engagement and decrease the amount of time spent sedentary.
Why have Flexible Seating?
Research on flexible seating has shown a great many benefit for both the student and the teacher leading the students. The list below attempts to encompass some of the research that has been done on the positive effects:
Increased focus and engagement
Increased self of control over environment
Creates a calm and FUN environment
Promote small group and large group work easily
Promotes physical activity and movement throughout the day
This increases blood flow and STIMULATES that growing brain!
Increases sensory input to help children with ADHD, ASD, etc.
Increased comfort while in a classroom setting
Physical therapy perspective on the benefits of Flexible Seating.
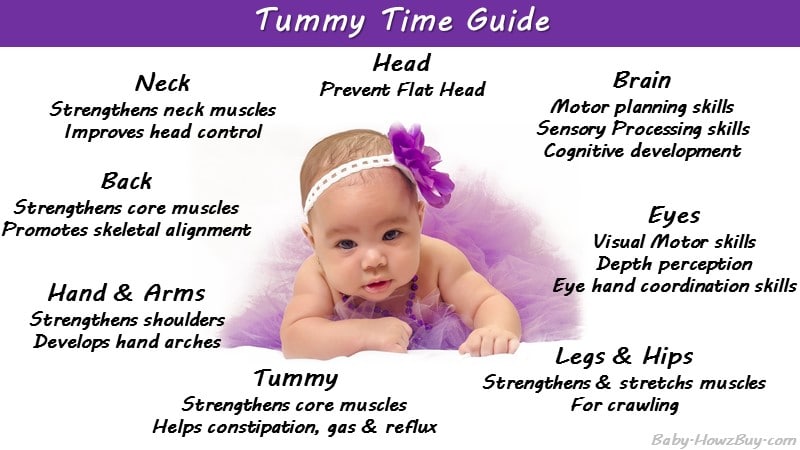
As a physical therapist I LOVE and excitedly promote flexible seating options for my clients (and their parents!) Humans are designed to MOVE not to be sedentary and flexible seating allows the body to find the motion it needs while still being able to attend to a cognitive task. Also, from a PT perspective, flexible seating = core strength and body awareness! These are some of the biggest things I work on with kids who need my services. Whether it is a child with Down Syndrome or a kiddo with Toe walking, I am constantly attempting to increase core strength as well as their perception of where they are in space. Flexible seating options allow them to explore this simultaneously as their brain is being empowered to learn more (WHAT A BETTER TIME TO IMPROVE INCREASED MOTOR FUNCTION?!) Check out some of these other benefits specifically related to physical activity and physical functioning:
Increased core strength
Decreased time spent sedentary
Decreased risk for cardiovascular/physical fitness decline
Decreased risk for childhood obesity
Increases calorie burn and metabolism
Increased balance
Increased sensory input
Could either be excitatory input to rev up the brain
Or inhibitory input to help calm and regulate in order to focus
the great part is the KID gets to chose what they need at that particular time!
Better posture
Less slouching, surfaces tend to promote more erect posture
Types of Flexible Seating
The following are types of flexible seating options that are commonly used in classrooms and could also be easily used inside of the home. I also included some ways to modify these for items you already have in your home and you didn’t know could be used to help improve your child’s focus! Follow the hyperlinks to see an example and where you can potentially purchase the products listed:
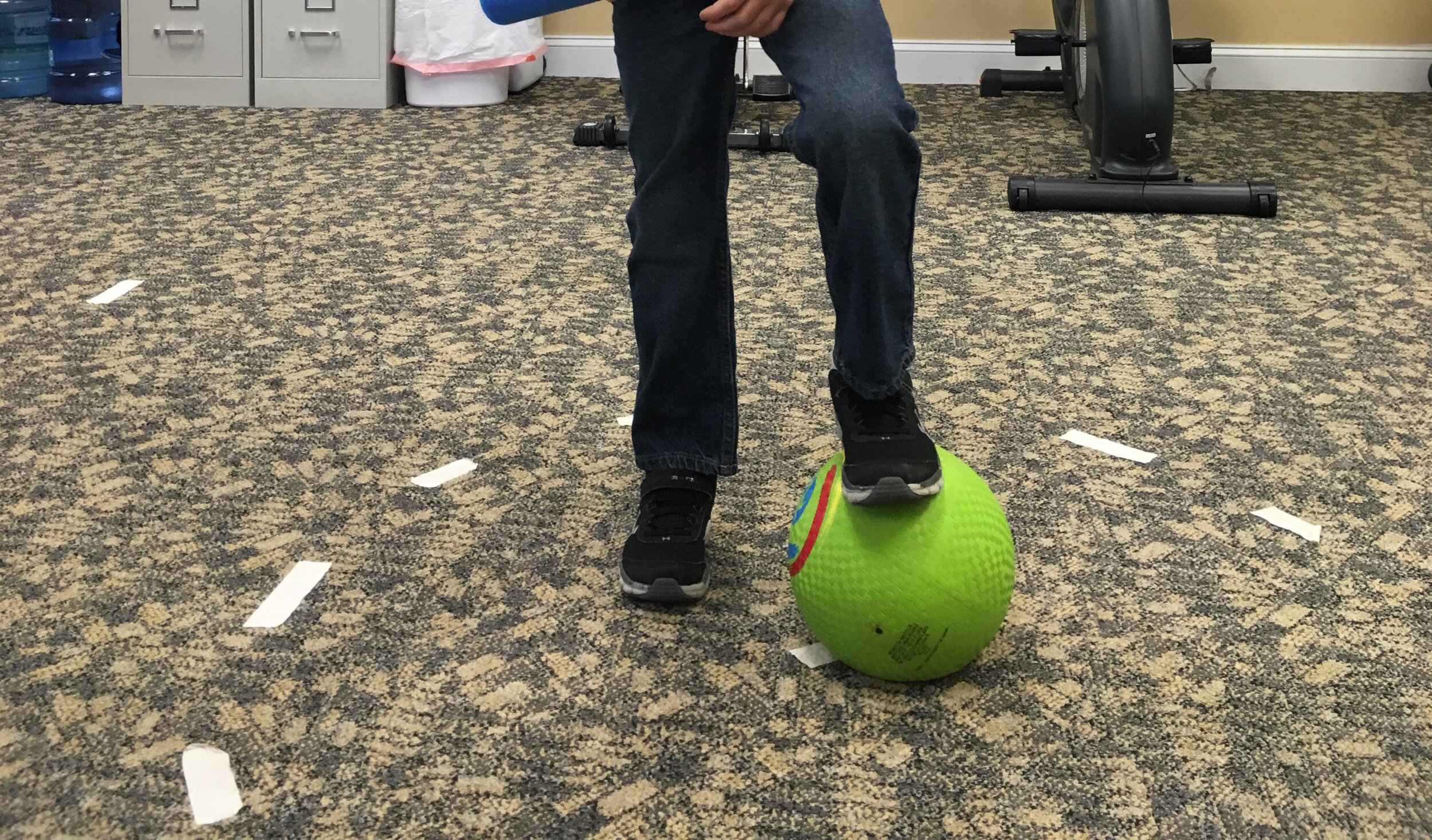
Balls
Wobbly seats
Floor Seating
Couch Cushions/pillows can be a great alternative to buying something
Standing Desk
Counter tops or Kitchen table (depending on child’s height) are a great way to modify this if you don’t want to purchase a standing desk
Seating Modifications
Do you have old resistance bands around your house?? You can tie these around the legs of a chair to simulate this!
You can also stand on this to modify a standing desk!
You can also stand on this to modify a standing desk!
Or sit on it on the ground!
Why should I use Flexible Seating in my Home?
If you are struggling to get your kid to concentrate I ask you to take a look at how you are making them sit for their work. Are they seated at the kitchen table on a chair that is too high for them, feet dangling? Are you allowing them to move around the house and work where they feel best?
Now I am not saying that they get to “work” right where all the games and distractions are but likely they haven’t found a new place that works best for them, and as a parent its your job to help guide them as their teacher would have to finding a place that makes them the most comfortable and able to concentrate. Kids are at home for the duration, this is their NEW classroom for at least now. Help them make the most of it!
Likewise, I ask you to ask yourself… what are YOU doing for your seating options? Are you now tele-working for the first time and finding your back hurts? Is your stiff at the end of the day? Are you fidgeting in a chair that is not really comfortable? It might be time to look at flexible seating options for you too! And there are a lot of great options that both you and your kid could benefit from! A rule of thumb I have for my adult clients is to only spend a maximum of 60 minutes in one position. After that time, switch positions or go for a walk if you can take a short break from your work… trust me on this! You’ll feel MUCH better.
And with that…Have fun with your Home-Classroom/Work Space Modifications!